Central Line Receiving Antibiotics Blood Draw
| Checking for a blood return is a significant component of a complete catheter patency assessment. Two standards of practice from the Infusion Nurses Society address this important step – Standard 61, Parenteral Medication and Solution Administration and Standard 45 Flushing and Locking. These statements do not limit the need to check for a blood return to a certain type of catheter or medication, making it important to obtain a blood return from both peripheral and central catheters prior to giving all medications. The reason for these standards is to prevent unnecessary complications such as infiltration or extravasation.
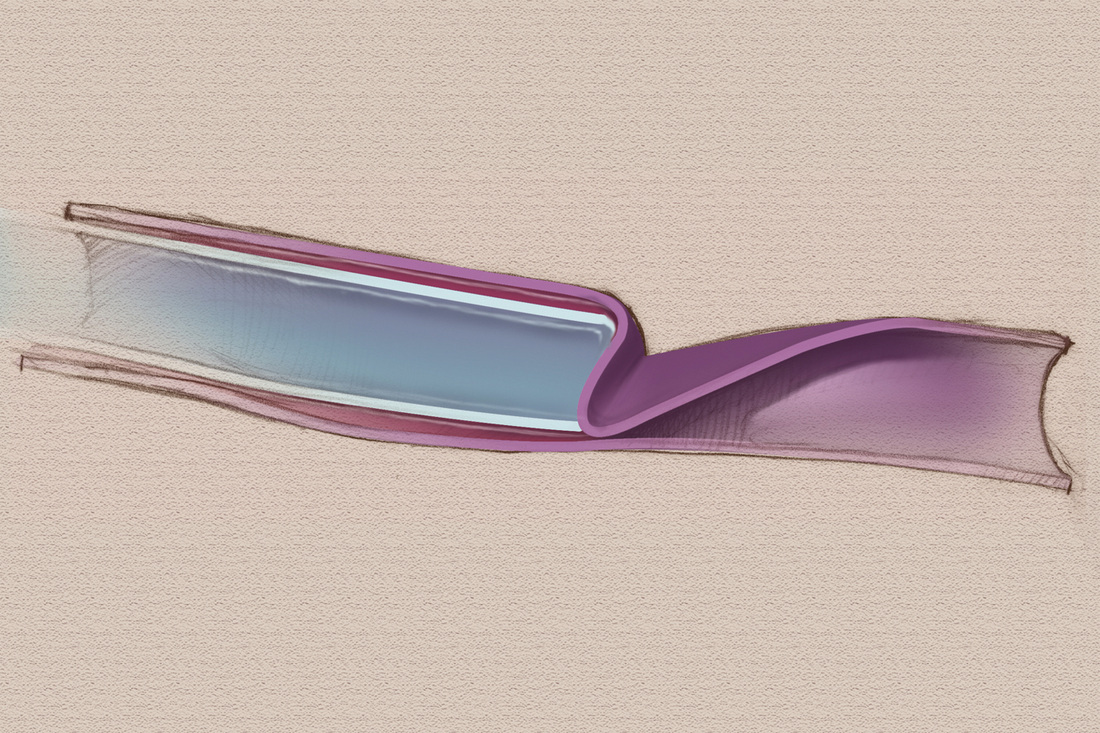
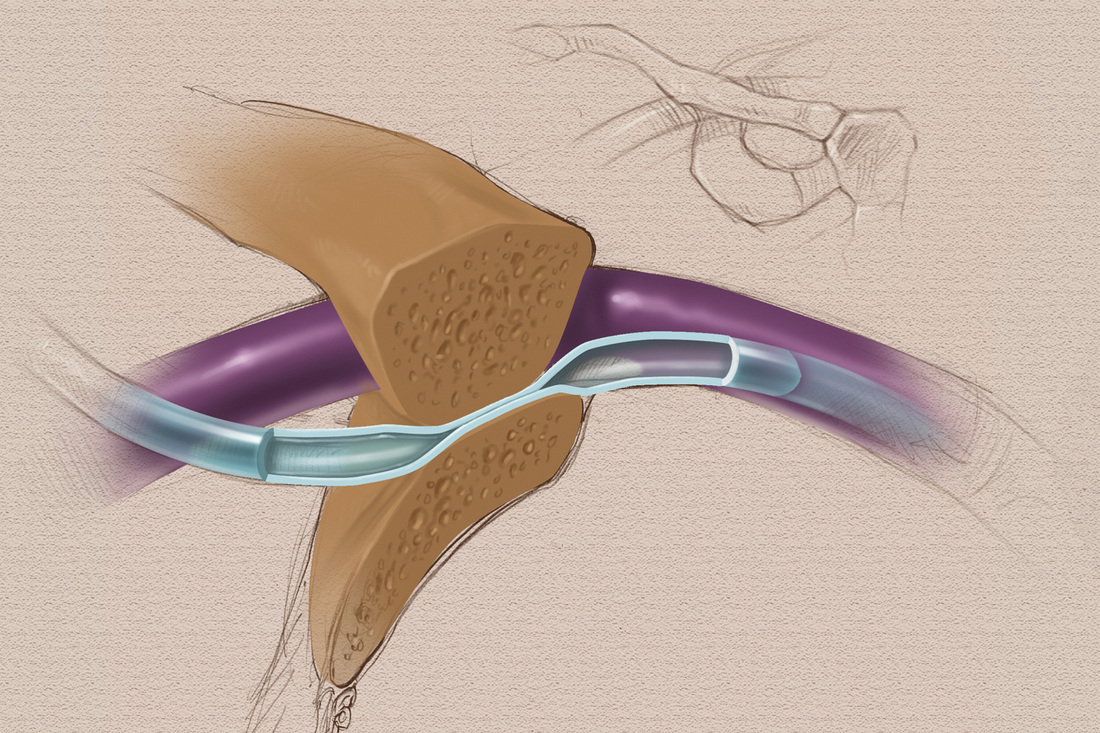
Collapsed peripheral vein wall occluding blood return Subclavian vein insertion with catheter pinched between clavicle and first rib Keith Gilchrist 2/5/2015 12:11:37 pm I was surprised to see the recommendation to use a smaller catheter gauge when attempting to aspirate as the smaller catheter will apply less pressure. I suppose as long as you don't flush with that smaller size catheter is ok, but I thought smaller catheters actually applied greater and could cause catheter rupture or thrombus dislodgement . I believe most IFUs and many standards and guidelines recommend only using 10ml and larger syringes, especially on CVADs. Jamie 2/10/2015 09:18:38 pm Yes you are mostly right. Smaller syringe size can cause You to place increase pressure, but has no effect when drawing. Vacuum is vacuum. You cannot exceed max vacuum by changing the syringe size. So this would have no effect. Changing the syringe size would only effect rate of volume. As far as using 10 ml syringes only, guideline stat that this is for establishing patiency Physics are physics When it comes down to pressure per square inch. And of course all of this is based on the strength of your thumb I may be able to profuse the same pressure with a ten cc syringe that you can produce with a three cc syring Lynn Hadaway 2/10/2015 11:32:41 pm Keith, I think you are referring to syringe size. You are correct about syringe size on INJECTION. But on aspiration, the opposite is correct. On aspiration a large syringe size has more surface area on the syringe, meaning that there can be greater force applied to pull the plunger rod. A smaller syringe will be more successful on aspirating a blood return for some situations and will not harm the catheter. In some PICCs, the force may cause a temporary collapse of the catheter and occlude the blood return, but the PICC returns to normal shape after the force is released. Also, on injection a 10 mL syringe is recommended for flushing, but when giving IV push medications, you must use a syringe size that is appropriate for the medication dose. Do not transfer the medication from a smaller syringe to a 10 mL syringe. This is included in the INS Standards on Flushing. Also a new paper from ISMP is now in the public comment stage and this paper will state similar things about syringe size and avoiding drug transfer. One other thing on syringe size for flushing - a 10 mL syringe is not the "safe harbor" that many may think. A strong hand on a 10 mL syringe flushing against resistance can cause catheter damage. Think about it this way - force applied to the syringe plunger rod meeting resistance along the fluid pathway can increase intraluminal pressure to the point of catheter damage. No resistance means the intraluminal pressure will not rise and there will be not catheter damage. So we can't rely only on syringe size. Nurses must understand the physics of what they are doing. Lynn, you explained inverse relationships and importance of tube radius, as it pertains to intraluminal volume and pressure; clearly and simply. I really appreciate all the work you do. Excellent. Keith 3/14/2015 03:14:02 am I'm still having a hard time wrapping my simple brain around this. I understand that aspirating is less likely to damage a catheter than flushing against an occlusion, so I'm not as worried about that. My hang up is just my experience of drawing blood from lines. It takes A LOT more muscle to draw blood into a large syringe than a small. Seems like the ratio of force required to pull is just as significant as that needed to push and they are both conversely proportional. I realize this discussion is now more about my misunderstanding of physics than infusion therapy, so I'll move on! Carolina Sachs 3/19/2017 12:17:12 am Using a smaller syringe (3-5 mL) produces higher psi than a 10 mL syringe. You should not try to aspirate with a syringe smaller than 10 mL This guideline is very useful. Medical students and even practitioners have always wondered how that can have been done better. The illustrations are also very clear. The instructions are precise. Please post more instructional articles like this. It's very useful for us. russ nassof 2/10/2015 12:53:04 am If more clinicians would read what Lynn publishes there would be fewer malpractice claims and the standard of care would improve. Thanks Russ. I sincerely wish we could stop the injuries that result in malpractice claims. Jackie Wallace 6/3/2015 11:46:59 pm My mother had MDS. She had a CBC twice a week to check to see if she needed platelets or red blood. This CBC was always taken from her arm. The last time she had a CBC, the nurse took it from her port. She had to flush it 3 times before it would draw. Her platelets were always extremely low. On this last day, from the time I took her across the waiting room to the doctor's office and into a room for a couple of minutes, she started having symptoms of a stroke and died later that day. I later learned her platelet count was 60 at the time her port was flushed 3 times. My question is this: Should there be a policy about not drawing blood from a port on an MDS patient with history of very low platelet count? The even sadder part of the story is that she was on an experimental treatment at MD Anderson that was working. It had started reducing her blasts. What a shock this was. Sona Mahal 2/10/2015 04:34:26 am I thought less than 10 ml syringe was not appropriate choice for a picc line. Please clarify. Thank you. Lynn Hadaway 2/10/2015 11:35:46 pm Sona, please read my reply to Keith above. Injection and aspiration are two different things. Robert Nohavec 2/10/2015 04:39:32 am Smaller catheters do create more pressure when you flush with them but it is the opposite when you aspirate. A 10 ml syringe generates more aspiration pressure than a smaller syringe. Lynn Hadaway 2/10/2015 11:36:14 pm Thanks Bob! Are your articles peer reviewed? Or are these written just off of your experience as an infusion specialist? Eve Nash, CRNI 11/4/2017 09:25:57 am Ashley, before posting this question (which could be construed as insulting, though I doubt Lynn is easily insulted) you should have done a search of her many infusion articles and the chapters of books she has written. Hers is one of the most respected names in infusion therapy, nursing, infusion research, infusion education. So... YES her stuff is frequently "peer-reviewed," though probably most often, in an attempt to learn from her! When we browse the net, we can have as lots of information instantaneously. Yet your own is the very best one. The provided information is really good and informative too. I have known many things about troubling in blood return. The procedures and techniques you have provided in article is very helpful for everyone. Thank you for sharing this problem with us. And a great solution as always! A writer should always try to keep its writing very simple and clear. Always use facts which are easily acceptable by general people because they are very close to their assumptions and they welcome such kind of facts. Real-time and placement focused Software Testing training in chennai determined to provide end-to-end Software Testing Training Course in Chennai for Students and Professionals Such a nice blog, Thanks for sharing this amazing information. Trendy doctor to provides natural medical tips, traditional medical tips, tradition secure life medical tips,siddha maruthuvam tips, Ayurveda medical tips, tradition health care, Traditional health care tips,unani maruthuvam tips, Traditional medical tips ,tradition medical solution, paarambariya maruthuvam tips, paddy maruthuvam tips, traditional health care solutions, natural health care, natural health care tips, health natural care, natural full medial solutions ,natural medical solutions, best natural medial tips Successful business occasion preparing requires a combination of skill, creativity, and effectiveness. No matter what type of business occasion you're preparing, the steps are basic and work efficiently for every occasion. It is amazing and wonderful to visit your site.Thanks for sharing this information,this is useful to me... Yvonne Rucker 8/6/2017 07:18:39 am I am trying to find a resource to show that smaller syringes exert less pressure when aspirating than larger syringes so that I can add it as a reference to a CVAD blood culture policy that I am creating. Could you provide that? I welcome all the suggestion mentioned in this blog related to new learning skills. It is definitely going to help me to adopt new exited way of learning. I think, others will also feel helpful this blog for their needs. thanx for shareing this informating blog Julia Carriere 12/4/2018 11:19:27 am I am a new Hickman user. I do my own administration of fluids daily. My problem is I have not been able to get blood return for two days now but the infusion goes in without any problems. How do I get blood return? I also have a catsan scheduled with contrast dye, can they still use it? There are many factors that should be included in an assessment of your tunneled cuffed catheter (eg, Hickman) that are not included in your message. These include the age of your catheter, exactly where the tip was located on insertion, changes in tip location determined by an X-ray, what fluids and medications have been given through the catheter, the amount and solution of flushing before and after each infusion. There are many things that could be causing this lack of blood return including a fibrin tail on the catheter tip acting like a valve, a partial or complete fibrin sheath, drug precipitate, the location of the catheter tip and a few other mechanical problems. The first step would be to obtain a thorough assessment of the catheter in radiology BEFORE your catheter is used for a CT scan. The absence of a blood return is a serious sign that a complication can happen. While a serious complication is not always guaranteed to occur, it is always better to be safe with this complete assessment before the contrast is injected of a CT scan. The management depends on what is found with this assessment. Before you have this radiology assessment, there are a few things you can check. If you are using a 10 mL syringe to attempt aspiration, use a very slow and gentle technique to pull back on the syringe plunger. Pulling back hard and fast can create this problem of absence of blood return. Next, change to a smaller syringe size, Instead of a 10 mL syringe use a 5 mL or a 3 mL sized syringe. On aspiration, smaller syringes created less pressure. Before aspirating, change the position of your arm and shoulder on the side where the catheter goes into the vein. Lift your arm up or pull your shoulder upward and backward. If this produces a blood return, make sure you tell this to the radiology staff. Good luck. What are those potential complications - infusion possible but lack of blood return? very nice nice blog keep sharing this type of blog Hello, nice and very easy to understand your blog CAROL GANNON 10/5/2020 08:33:18 am MY HUSBAND HAS INFUSION PORT FOR FOUR YEARS AND GET SALINE TWICE A WEEK - ALL OF A SUDDEN NURSE CANNOT GET BLOOD DRAWN BUT OTHER DAY NURSE WAS ABLE TO DO SO USING COUGHING TECHNIQUE - TODAY IT HAPPENED AGAIN WHAT CAN BE DONE INSTEAD OF PUTTING NEW LINE IN...... CAROL GANNON 10/7/2020 03:43:20 pm COULD PORT HAVE LEAKAGE - HE IS GOING FOR TEST TOMORROW MEDS INSERTED TO SEE WHAT THE PROBLEM COULD BE...... Mais India is iv cannula exporter and we also provide our iv cannula and other medical disposable product in all over the world because we are manufacturer of medical disposable products and our products are very good quality because our team mainly focus on the quality of a product. Hi Thanks a lot very much for the interesting article. Anyone who purchase Medical Equipment visit us at. https://www.larsmedicare.com/iv-cannula-exporter-manufacturer-supplier/ Leave a Reply. |
Central Line Receiving Antibiotics Blood Draw
Source: https://hadawayassociates.com/lynns-blog/trouble-getting-a-blood-return


 RSS Feed
RSS Feed
0 Response to "Central Line Receiving Antibiotics Blood Draw"
Post a Comment